“Normalcy”, “Normality”, “Normal”; No more. I’ve never heard the verbal and written abuse of a seemingly, well, normal, word as much as the six-letter description of what is supposed to be over the past three months. For those of us familiar with the U.S. healthcare system, we’ve discarded the word “normal” from our vocabulary long ago.
As many of us anxiously await the “end” of the most recent global pandemic one common phrase has stood out among healthcare industry experts as the most detrimental aspect of the recent outbreak: “overwhelming the healthcare system.” In short, overwhelming the healthcare system can be illustrated by imagining the hospitals in our areas completely overrun with so many COVID diagnoses that it affects the ability for facilities to manage and effectively treat regular hospital patients (not spurred by the pandemic) resulting in worsened health outcomes for all. Luckily, we will avoid a blanketed overwhelming scenario in the U.S. due to this pandemic, but that doesn’t relieve the concern of a looming explosion of chronic illness that is likely to take a similar path within the American population.

The Potential Impacts of Overwhelming Chronic Illness on the U.S. Healthcare System
For the remainder of this post, we’ll isolate one of these chronic illnesses to get an idea of what overwhelming our healthcare system with chronic illness would look like financially. In its various forms, this illness affects, has affected, or will affect approximately 152.3 million Americans. Of those 152.3 million individuals:
- 68.3 million are currently diagnosed, previously have been diagnosed, or have the disease but have yet to be officially diagnosed
- 84 million are in a “pre-disease” situation where they are at high risk of being diagnosed or are on a quick path to the fully blown disease
- 90 percent of those 84 M in the pre-disease stage aren’t even aware they’re at risk
To put these numbers into perspective, below is a graph comparing the number of COVID-19 diagnosis in the United States (as of 4/25/20) vs. the aforementioned chronic illness:
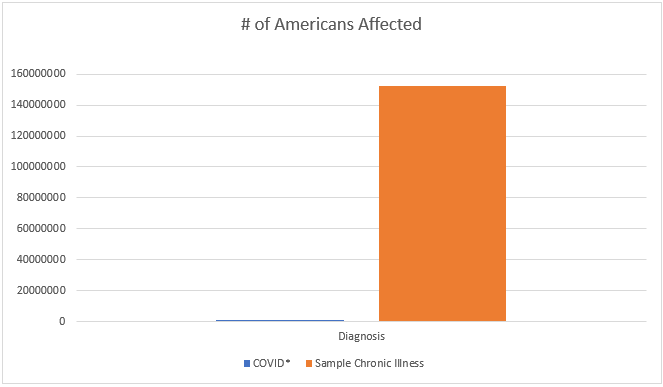
From sheer diagnosis numbers alone, this chronic illness should appear way more drastic to our hospital system than our current pandemic (obviously, the numbers surrounding COVID are subject to change as we learn more). This would assume that all diagnosed patients end up in our hospital system which isn’t a guarantee. To compensate for that lack of future clinical data, we’ll substitute what we know from a financial aspect on how impactful this chronic disease could be to our HC system. To do this I’m going to use some “creative” arithmetic. Bear with me.
A Hypothetical Financial Projection
To try and make this as accurate as possible, we’re going to take inflation into account. To do so, we’ll use the generation markers for Baby Boomers (55 – 76 years old) as a starting point for our projection. The financial data surrounding this chronic illness is largely from 2017 so we’ll use three years of inflation projections to get us into 2020 USD, and then another 21 years of projections to completely age-out the current Baby Boomer population (ending in 2041).
From 2017 – 2020 we’ve experienced about $0.05 in inflation. Now, unrealistically, we’re going to assume that every three years we will continue to have a $0.05 inflation hike. This projection would put the U.S. at a $0.35 inflation hike between 2020 and 2041.
Now we can apply our existing data. According to an organization specializing in this disease, $327 billion is spent annually to treat those diagnosed. Referencing our population data, those diagnosed represents a small minority of those likely to develop the disease as a whole: 34.2 million diagnoses vs. 152.3 million diagnoses, pre-diagnoses, and former diagnoses. If we can break down our data to represent the cost of an individual diagnosis, we can then scale for inflation and a more accurate financial point to include all of those at risk, not just those who have been officially diagnosed. Here’s the math step by step:
- $327 Billion spent in 2017 for all American Diagnoses * 1.05 = $343.35 Billion USD in 2020 currency (1.05 represents the inflation rate between 2017-2020).
- $343.35 Billion (2020 Dollars) * 1.35 = $463.5225 Billion (2041 Dollars – Assuming we see a $0.05 inflation hike every 3 years between 2020 and 2041).
- $463 Billion dollars is a huge chunk of change even on a national scale. What this figure doesn’t include are the pre-diagnosed, un-diagnosed, and formerly diagnosed Americans that are at a higher likelihood to develop or re-develop the disease. This $463 Billion figure represents only 34.2 million of the 152.3 million Americans at risk:
- $463,522,500,000 / 34,200,000 diagnosed = $13,553.29 per diagnosis per year. It’s important to keep in mind that these costs are the total impact on the healthcare system.
- $13,553.29/diagnosis * 152.3 Million Americans at risk = $2.064 Trillion per year in theoretical financial impact towards the US healthcare system in 2041 for this chronic illness.
If you’re still wondering which chronic illness we’ve used to project these outcomes, it’s Diabetes Mellitus. These figures represent solely the cost of treating diabetes itself (insulin, test strip, A1C monitors, physician services, glucose monitors, etc.), not the complications that can stem from the disease. Some common complications are stroke, heart disease, neuropathy, eye and skin complications (like glaucoma and deep skin infections or sepsis), etc.
These numbers are meant to be staggering. This is a projection for one chronic illness out of hundreds, with hundreds more to be developed or contracted between now and 2041. If our healthcare system was at the brink of being overwhelmed during the COVID pandemic, what capacity can we expect the system to hold for a chronic illness that will affect 197.58 percent more Americans and cost billions if not trillions of dollars? The good news, type II Diabetes (a heavy, heavy majority of diabetes diagnoses statistics) is reversible through proper medication, diet, exercise, and lifestyle changes. The bad news? Many other chronic illnesses are not.
Steps for a Sustainable Healthcare System
If this pandemic has shown us some shortfalls within our healthcare system, now is the time to correct them. Individual education and individual ownership of lifestyle choices are immediately impactful changes we can all make to ensure the healthcare system is sustainable for future generations. If we can successfully manage our own health, we won’t need to rely on a potentially ineffective healthcare system.
Contact GMS to discuss how we are partnering with local businesses to control and stabilize their healthcare programs for years to come. Our industry experts are prepared to discuss the future of healthcare and how it may affect your business, your employees, and you.